Is Opioid Replacement Therapy really safe? That’s a difficult question, with shades of grey when it comes to the definition of “safe.” To answer the question fully, let’s examine the practice of opioid replacement therapy more closely.
If you have question about opioid addiction treatment, call us today at 888.296.8976.
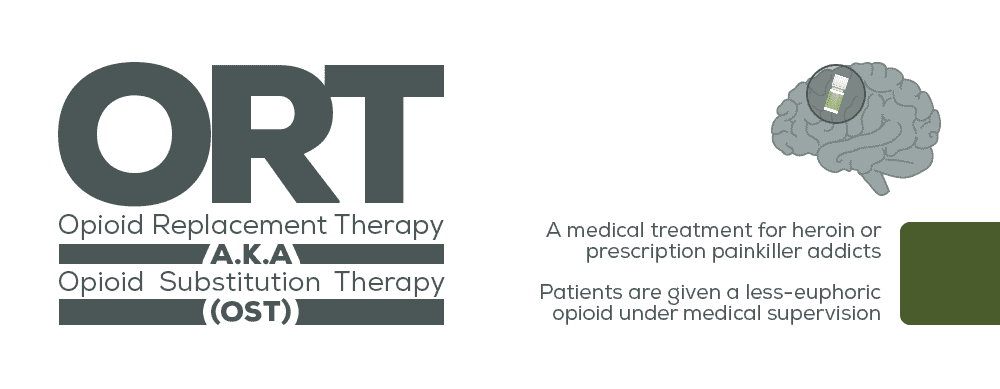
What is Opioid Replacement Therapy?
Opioid Replacement Therapy (ORT) is a medical treatment of opioid addiction where a patient suffering from a heroin or prescription painkiller addiction receives a less-euphoric opioid under medical supervision. It can also be referred to as Opioid Substitution Therapy, or OST.
The two most-commonly-prescribed medications are methadone and buprenorphine. When prescribed and taken correctly, each of these medications ease withdrawal symptoms and reduce cravings. However, they DO come with certain limitations and risks.  The idea of using “safer” opioids to treat opioid addiction is based on the idea that chronic drug abuse profoundly alters the user’s brain. The cravings, drug-seeking, and abuse of opioids becomes a “bio-behavioral” compulsion. Proponents believe that replacing dangerous illicit drugs with safer legal ones and dirty needles with medically-dispensed pills, films, and liquids reduces the harm to both addicts and society.
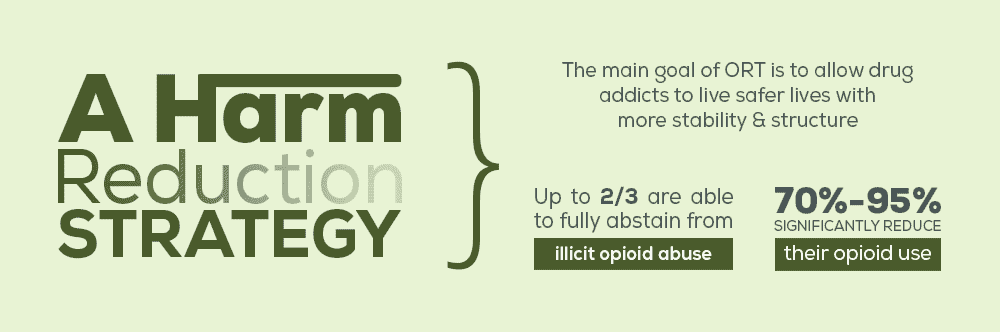
The idea of using “safer” opioids to treat opioid addiction is based on the idea that chronic drug abuse profoundly alters the user’s brain. The cravings, drug-seeking, and abuse of opioids becomes a “bio-behavioral” compulsion. Proponents believe that replacing dangerous illicit drugs with safer legal ones and dirty needles with medically-dispensed pills, films, and liquids reduces the harm to both addicts and society.  ORT’s main focus is NOT specifically to enable the patient to live a completely drug-free life. Rather, it is to allow the former drug-addicted individual to live a safer life, one with a greater degree of stability and normalcy. This is why ORT is a “harm reduction” strategy. For those patients who are motivated to move totally away from drugs, their medication can be very gradually tapered, while other types of methadone addiction treatment are utilized.
ORT’s main focus is NOT specifically to enable the patient to live a completely drug-free life. Rather, it is to allow the former drug-addicted individual to live a safer life, one with a greater degree of stability and normalcy. This is why ORT is a “harm reduction” strategy. For those patients who are motivated to move totally away from drugs, their medication can be very gradually tapered, while other types of methadone addiction treatment are utilized.
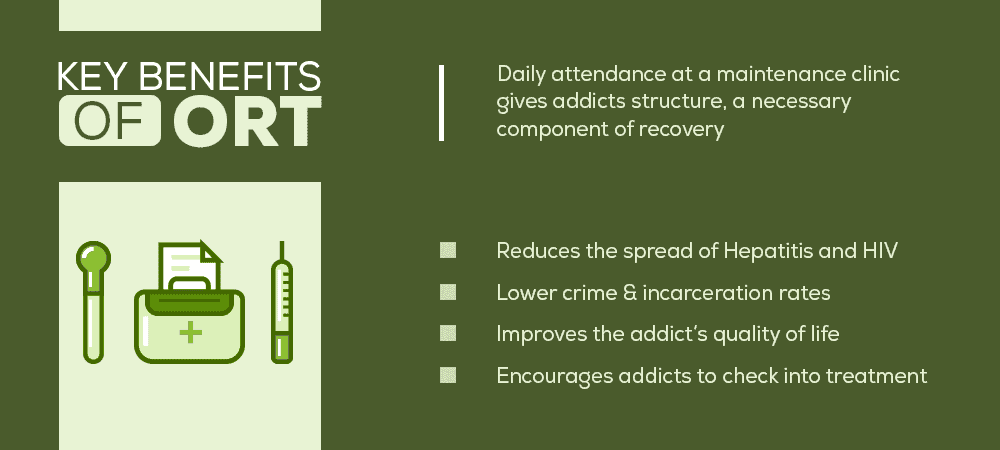
Benefits of Opioid Replacement Therapy
The World Health Organization, the Substance Abuse and Mental Health Services Administration, the United Nations Office on Drugs and Crime, and the Joint United Nations Program on HIV/AIDS all support ORT. ORT gives opioid addicts a chance to gradually wean from other, more dangerous opioids without experiencing debilitating withdrawal symptoms. Other ways that ORT reduces harm include:
- Up to two-thirds of opioid addicts receiving ORT are able to totally abstain from illicit opioid abuse
- 70%–95% significantly reduce their opioid use
- Medically-assured purity, quality, and dosage
- Reduces the spread of Hepatitis and HIV, because it allows IV drug abusers to stop using needles
- Encourages drug addicts to enter drug treatment programs
- Lower crime and incarceration rates
- Improves quality of life and the ability to hold a job, maintain relationships, etc.
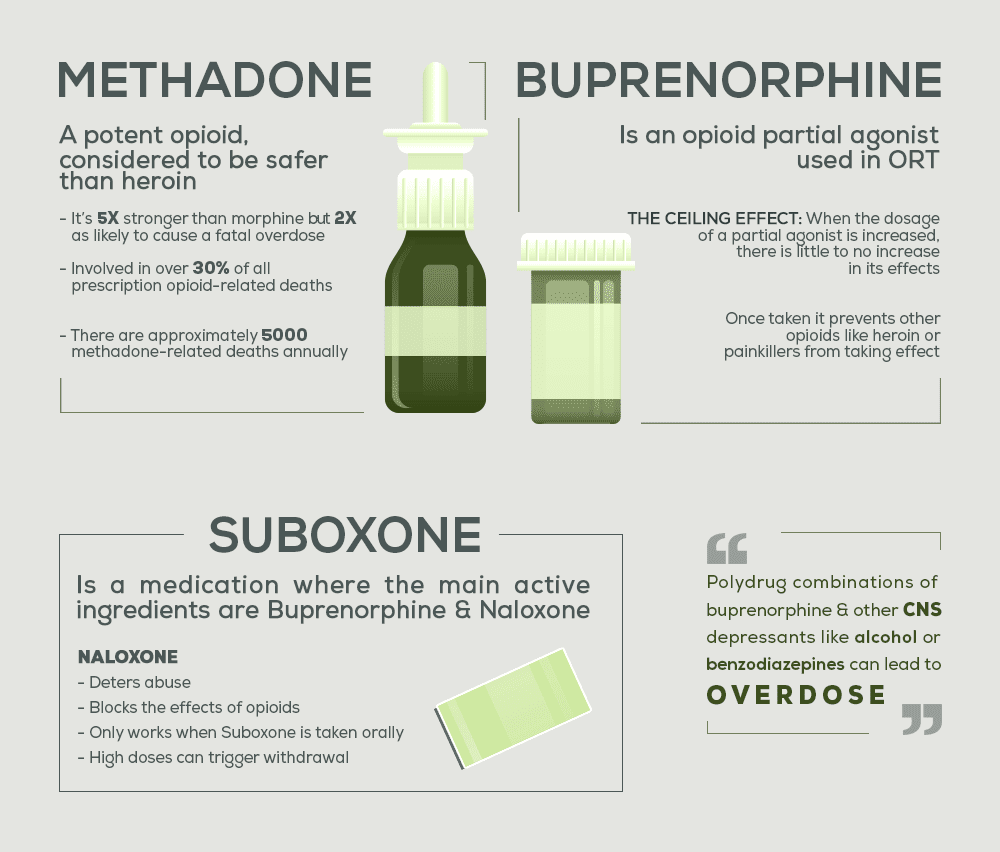
Methadone – the Risks
Healthcare professionals consider methadone safer than heroin. However, it is an extremely potent opioid—five times stronger than morphine—that carries risks all its own:
- Methadone accounts for just 2% of all opioids prescribed for pain, but is involved in over 30% of all prescription opioid-related deaths
- Methadone is four times more likely to cause a fatal overdose than oxycodone
- It is twice as likely to cause a fatal overdose as morphine
- 40% of single-drug prescription overdose deaths are because of methadone
- In 1999, 790 people died because of methadone
- Today, there are approximately 5,000 annual deaths due to methadone use
Buprenorphine: A Better Alternative?
Buprenorphine is rapidly increasing in popularity as a ORT medication. In 2014, 60%–65% of patients receiving any medication-assisted treatment were prescribed buprenorphine, either alone or with naloxone, in a combination product called Suboxone. Most experts expect that number to rise sharply in the future.
A Few Words About Suboxone
The addition of naloxone in this formulation helps deter abuse. In fact, at high doses, Suboxone can trigger withdrawal in someone addicted to opioids. According to the US Institute on Drug Abuse, Suboxone is a first-line treatment medication for opioid dependence. However, there is a caveat—the naloxone in Suboxone is only effective when patients take the medication orally. If the drug is misused intravenously, the naloxone is not metabolized, resulting in an opioid high.
This is a legitimate concern, because Suboxone is prescribed for at-home use, unlike methadone. Patients taking methadone at a clinic must demonstrate a significant period of sobriety and program adherence, before there is even a possibility of a take-home prescription.
Advantages of Buprenorphine
Even though buprenorphine is far more potent than methadone—up to 30 times stronger than morphine—it is a partial-agonist, giving it several advantages over methadone, a full agonist. Whereas the effects of methadone increase with dosage, buprenorphine’s affects level off at a plateau, meaning it has a “ceiling affect” that does not increase, even with increased dosage.
In other words, a person given buprenorphine cannot get high from any opioid. This is key when it comes to preventing overdose deaths.
Limitations of Buprenorphine
The biggest criticism of buprenorphine is the fact that its ceiling effect means that at low doses, it is not as effective as methadone at satisfying the cravings and withdrawal symptoms experienced by individuals who are accustomed to very high doses of heroin. At medium and higher dosages, however, buprenorphine and methadone are equally effective.
Of Special Interest to Pregnant Women
Among pregnant heroin abusers, buprenorphine abuse to be a much safer option for ORT than methadone. One study shows that compared to methadone, buprenorphine ORT results in:
- Longer gestation
- Higher birth weight
- Shorter hospital stays
- A much lower incidence of neonatal abstinence syndrome (NAS) – 40% versus 78%
- Of those infants born with NAS, only 15% of those whose mothers used buprenorphine needed withdrawal treatment, while 53% of those whose mothers used methadone did
Moving On from ORT
One of the most profound differences between using either methadone or buprenorphine during ORT is the fact that it’s possible to discontinue buprenorphine at any time. In contrast, methadone dosages require a slow reduction. This has strong implications for anyone who wants to move forward in recovery completely substance-free.
ORT, like any form of medication-assisted treatment, is a valuable recovery tool for those who need it. However, for those with a motivation to achieve total abstinence, ORT should only serve as temporary support, until they are able to stay sober on their own.
If you’re suffering from opioid addiction, don’t wait to seek help. To learn about your opioid treatment options, call Northpoint Idaho today at 888.296.8976 for more information.
What Did you Think About This Blog?
Give it a Rating!
Full Infographic:
 https://pcssmat.org/wp-content/uploads/2015/10/Mortality-Risk-Methadone-buprenorphine-Kimber-2015-Lancet-Psychiatry.pdfhttps://www.bmj.com/content/357/bmj.j1550https://www.cdc.gov/mmwr/volumes/66/wr/mm6612a2.htmhttps://www.cbsnews.com/news/methadone-to-blame-for-one-third-of-us-prescription-painkiller-deaths-cdc-says/https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2015/4/23/most-states-list-deadly-methadone-as-a-preferred-drughttps://www.bmj.com/content/344/bmj.e2823https://europepmc.org/articles/PMC2842557/https://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdfhttps://www.cdc.gov/mmwr/preview/mmwrhtml/mm6149a1.htmhttps://www.bmj.com/content/357/bmj.j1947https://www.sciencedaily.com/releases/2016/05/160502111242.htmhttps://www.justice.gov/archive/ndic/pubs10/10123/index.htmhttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC2874458/https://www.ncbi.nlm.nih.gov/pubmed/11452842/https://www.nytimes.com/2013/11/17/health/in-demand-in-clinics-and-on-the-street-bupe-can-be-savior-or-menace.htmlhttps://www.ncbi.nlm.nih.gov/pubmed/18355989https://www.cochrane.org/CD002207/ADDICTN_buprenorphine-maintenance-versus-placebo-or-methadone-maintenance-for-opioid-dependence
https://pcssmat.org/wp-content/uploads/2015/10/Mortality-Risk-Methadone-buprenorphine-Kimber-2015-Lancet-Psychiatry.pdfhttps://www.bmj.com/content/357/bmj.j1550https://www.cdc.gov/mmwr/volumes/66/wr/mm6612a2.htmhttps://www.cbsnews.com/news/methadone-to-blame-for-one-third-of-us-prescription-painkiller-deaths-cdc-says/https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2015/4/23/most-states-list-deadly-methadone-as-a-preferred-drughttps://www.bmj.com/content/344/bmj.e2823https://europepmc.org/articles/PMC2842557/https://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdfhttps://www.cdc.gov/mmwr/preview/mmwrhtml/mm6149a1.htmhttps://www.bmj.com/content/357/bmj.j1947https://www.sciencedaily.com/releases/2016/05/160502111242.htmhttps://www.justice.gov/archive/ndic/pubs10/10123/index.htmhttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC2874458/https://www.ncbi.nlm.nih.gov/pubmed/11452842/https://www.nytimes.com/2013/11/17/health/in-demand-in-clinics-and-on-the-street-bupe-can-be-savior-or-menace.htmlhttps://www.ncbi.nlm.nih.gov/pubmed/18355989https://www.cochrane.org/CD002207/ADDICTN_buprenorphine-maintenance-versus-placebo-or-methadone-maintenance-for-opioid-dependence