Prescription medication abuse and addiction rates have soared across the U.S. over the past few years. Many people are familiar with the opioid epidemic, which focuses on addictions to painkillers made from natural and synthetic opium. However, other medications can also be highly addictive and cause people to easily become mentally and physically dependent on them. Benzodiazepines, or benzos, are one of these addictive prescriptions.
At Northpoint Recovery, we know how difficult it can be to break the addiction cycle. Our benzo addiction treatment program can help you get sober and learn how to live a life without drugs. Call 888.296.8976 today to speak with a recovery specialist about your enrollment options.
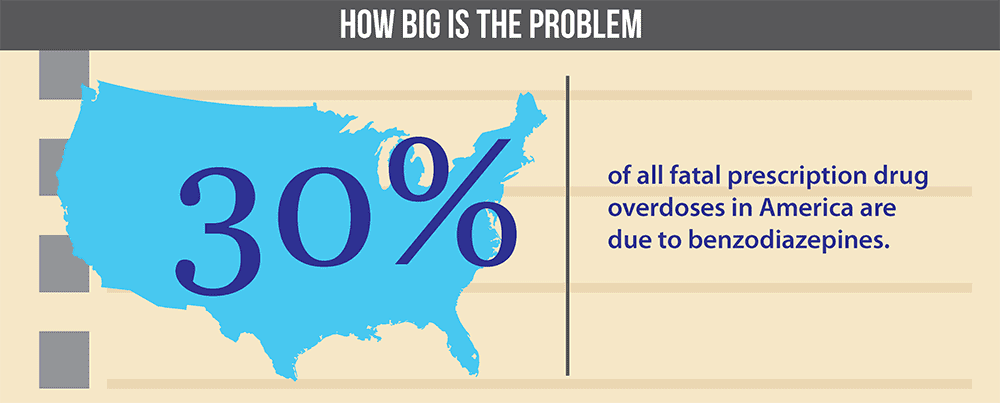
How Big Is the Problem?
Every year, millions of prescriptions for benzos are written in the U.S. These drugs are designed to treat anxiety, insomnia, and seizure disorders. Their effects can be calming and relaxing, which is why they’re often used as a way to deal with stress.
However, benzos are also highly addictive. More than 30% of people who take them will develop an addiction. And once someone is addicted, it can be challenging to break free from the addiction without professional help.
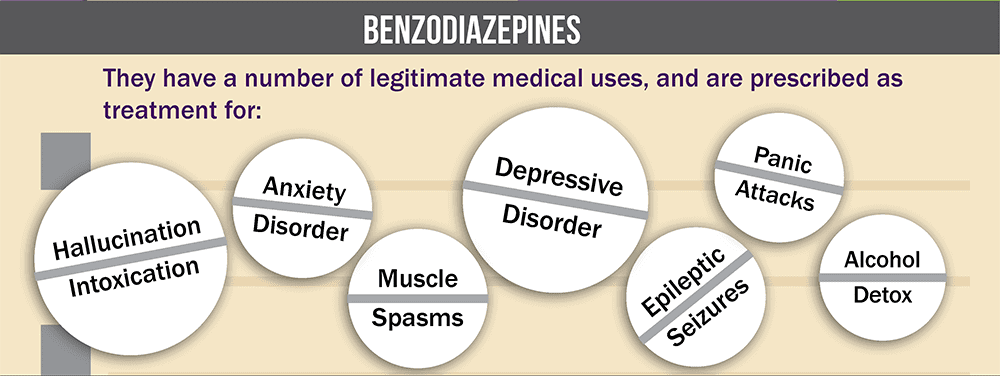
What Are Benzos?
Benzos are central nervous system depressants. This effect means they slow down the brain and the body’s systems.
These drugs work by binding to gamma-aminobutyric acid (GABA) receptors in the brain. GABA is a neurotransmitter that helps regulate the nervous system. When benzos bind to GABA receptors, it decreases the body’s overall activity level. This effect can lead to feelings of relaxation and drowsiness.
Benzos are generally only meant to be taken for a short period because they can easily lead to tolerance, dependence, and addiction. Tolerance occurs when a person needs to take larger doses of the drug to achieve the same effects. Dependence happens when a person’s body becomes used to the drug and begins to experience withdrawal symptoms when they try to quit. And addiction is a chronic disease characterized by compulsive drug-seeking behaviors, despite the negative consequences.
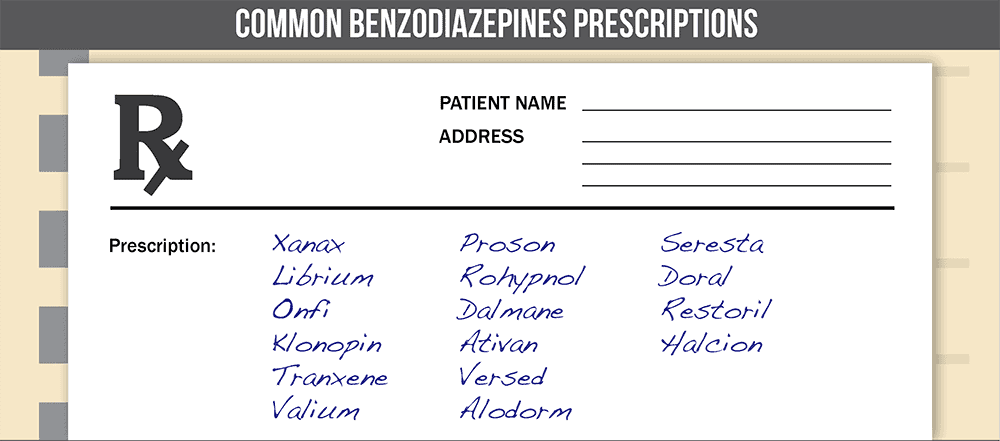
Commonly Prescribed Benzo Medications
There are several different types of benzos that physicians prescribe in the U.S., including:
- Alprazolam, sold as Xanax
- Chlordiazepoxide, sold as Librium
- Clonazepam, sold as Klonopin
- Diazepam, sold as Valium
- Lorazepam, sold as Ativan
These drugs help treat anxiety, insomnia, and seizure disorders. They’re also sometimes used to help people detox from alcohol because they can reduce the symptoms of withdrawal. However, like many other drugs, they come with the risk of harmful side effects.
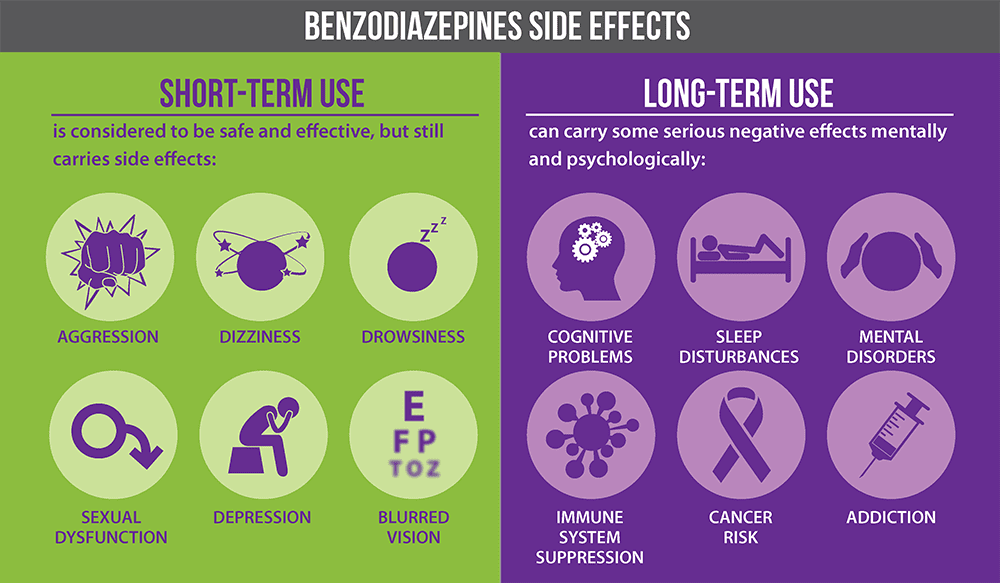
Benzodiazepine Side Effects
Short-term side effects of taking benzos can include:
- Drowsiness
- Confusion
- Memory problems
- Slurred speech
- Weakness
- Poor coordination
People who struggle with benzo addiction may experience the long-term side effects of the drugs like anxiety, depression, paranoia, psychotic episodes, blurred vision, difficulty urinating, and muscle weakness.
Why Are Benzodiazepines Addictive?
Benzodiazepines are some of the most commonly abused drugs in the U.S. In fact, they’re involved in more overdose deaths than any other type of prescription medication.
There are a few reasons why these drugs are so addictive. For one, they’re very easy to access. Many people have them prescribed for legitimate reasons. And once someone has a prescription, it’s easy to get more of the drug, either by getting another prescription or buying them from someone else.
Another reason benzos are so addictive is that they’re very effective at treating anxiety and other mental health disorders. When taken as prescribed, they can be helpful for people who struggle with these conditions. But because they’re so effective, it’s easy for people to start using them in larger doses or more often than they should.
Withdrawing from Benzos
When someone addicted to benzos tries to quit, they may experience withdrawal symptoms. These symptoms can include:
- Anxiety
- Insomnia
- Muscle tension
- Nausea
- Vomiting
- Sweating
- Tremors
- Seizures
- Paranoia
- Psychosis
Withdrawal from benzos can be very dangerous, and it’s important to detox under the care of a medical professional.
Benzo Addiction Treatment at Northpoint Recovery
If you or someone you love is struggling with benzo addiction, we can help. At Northpoint Recovery, we offer comprehensive treatment programs designed to meet each patient’s unique needs.
Our programs include:
- Medical detox
- Inpatient treatment
- Relapse prevention
To learn more about our program and get started on the road to recovery, call 888.296.8976 today.