If you’ve struggled with addiction or watched someone close to you go through it, you may have wondered if it “runs in the family.” Science shows that addiction does have a genetic component, but it’s not the whole story. While family history can raise your risk, it doesn’t guarantee you’ll develop an addiction yourself.
Here’s what we know.
Genetics Play a Big Role — but Not the Only One
According to the National Institute on Drug Abuse (NIDA), genetic factors account for 40–60% of a person’s risk for developing a substance use disorder. That means some people may be born with a higher likelihood of becoming addicted if they use drugs or alcohol, especially if they have close relatives who’ve struggled with it.
That risk comes from a combination of inherited traits. Some people may be more sensitive to the effects of certain substances, more prone to impulsivity, or more likely to use drugs as a way to cope with stress, all of which can increase vulnerability.
But even with a high genetic risk, environment and personal choices still matter a lot.
Other Addiction Risk Factors (Besides Genetics)
Even without a family history of addiction, certain experiences and traits can raise your risk. These aren’t about weakness or bad choices—they’re about how the brain responds to stress, reward, and relief.
Below are some of the most common non-genetic risk factors, explained in full:
Early Exposure to Substances
Using drugs or alcohol at a young age, especially during the teen years, can rewire the brain in a way that makes it easier to develop a dependency later. The brain is still developing during adolescence, and exposure to substances during this time can interfere with normal reward processing and impulse control. That can lead to stronger cravings, faster escalation of use, and greater difficulty quitting later in life.
Unresolved Trauma
People who’ve lived through trauma, especially ongoing or repeated trauma like abuse, neglect, or violence, are more likely to develop addiction. That’s because substances can offer temporary relief from overwhelming emotions, flashbacks, or numbness. Over time, the brain begins to associate the substance with safety or escape, making it harder to stop. Without treating the underlying trauma, the drive to self-medicate often remains strong.
Chronic Stress
Stress on its own doesn’t cause addiction, but it does increase vulnerability. When the brain is constantly in fight-or-flight mode, it craves relief. Substances like alcohol, opioids, or stimulants can feel like a quick way to calm down or feel in control. The more someone uses that shortcut, the more likely it is to turn into a dependency, especially if they don’t have healthy coping tools in place.
Co-Occurring Mental Health Disorders (Dual Diagnosis)
Anxiety, depression, PTSD, ADHD, and other mental health conditions can significantly raise the risk of addiction. In many cases, people turn to substances to manage symptoms, trying to feel less anxious, more focused, or simply more numb. This cycle of self-medication can make both conditions worse. Untreated mental health issues can also make recovery harder if they’re not addressed at the same time as substance use.
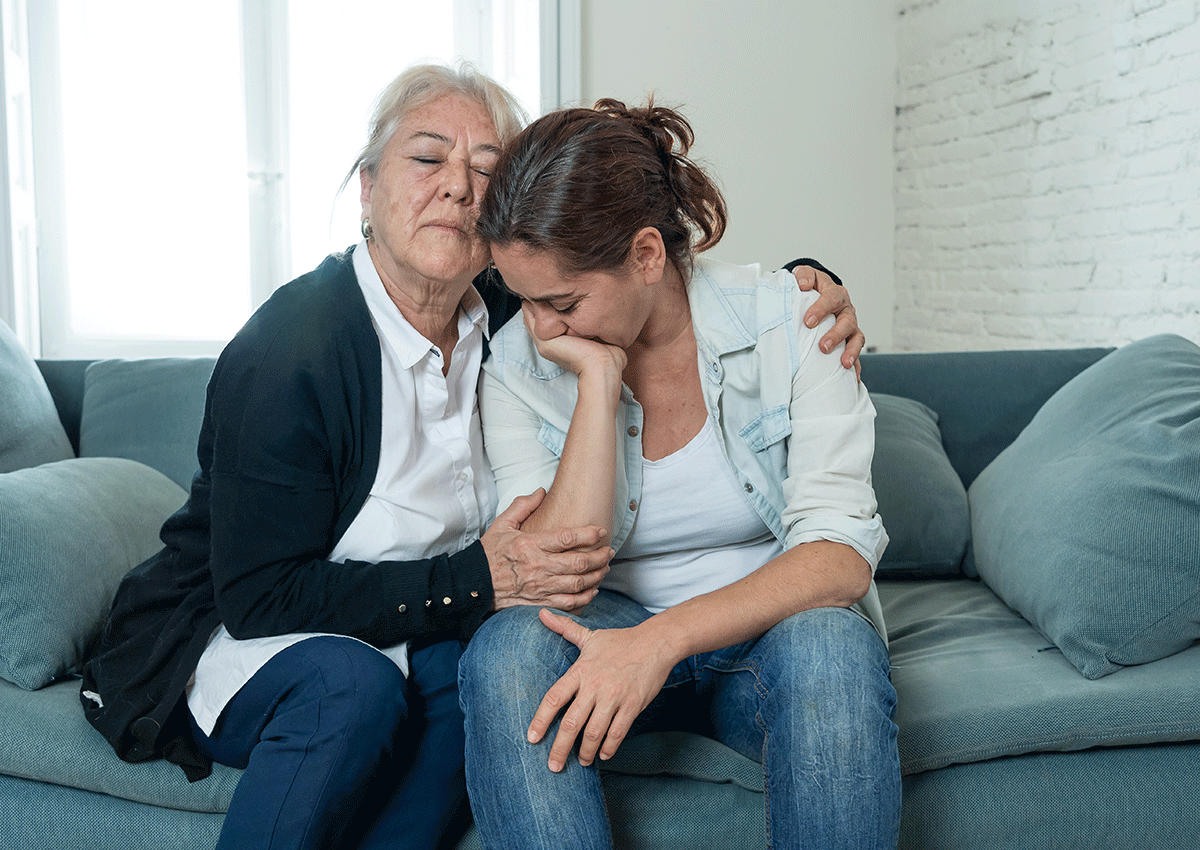
Lack of Support or Connection
Isolation doesn’t always cause addiction, but it does make it more likely to take hold. People without strong social support, whether that’s family, friends, or a recovery community, may have a harder time managing stress or finding healthier ways to cope. On the flip side, connection is one of the strongest protective factors. Feeling seen, supported, and understood helps reduce the need to use substances as a way to cope.
Understanding Addiction Risk Factors and What They Look Like
When people hear the term risk factor, it can sound vague or overly clinical. But it’s actually pretty straightforward. A risk factor is anything that increases the chances that someone might develop a substance use disorder.
Risk factors aren’t guarantees. They don’t mean you will develop an addiction; they just mean the chances are higher, especially if multiple factors are present at the same time. Think of them like weights on a scale. The more that pile up, the easier it becomes to tip into unhealthy patterns.
Addiction Risk Factors in Context: Real-Life Examples
Example 1: Stress Without Support
Let’s say someone has a high-pressure job and feels burned out, but doesn’t have many close relationships or ways to manage stress. Over time, they might start drinking every night to take the edge off. At first it works—until it starts interfering with sleep, relationships, or mood. That’s a pattern that can lead to dependency, even without a family history of addiction.
Risk factors involved:
- Chronic stress
- Lack of social support
- Using substances to cope
Example 2: Past Trauma and Emotional Numbing
Someone who experienced childhood abuse might struggle with anxiety and emotional regulation. They discover that painkillers or benzos help them feel calm or disconnected from the pain. Over time, those substances can become the go-to escape, and eventually, the brain starts craving that escape just to feel “normal.”
Risk factors involved:
- Unresolved trauma
- Mental health challenges
- Emotional avoidance
Example 3: Early Substance Use With a Genetic Link
A person starts drinking heavily in high school, and it becomes part of how they socialize or cope with pressure. Their dad also struggled with alcohol, but they’ve never talked about it. Years later, they notice they’re drinking daily and feel irritable or anxious without it. That early exposure, combined with inherited risk, increases their chances of addiction.
Risk factors involved:
- Family history of addiction
- Early exposure to alcohol
- Learned behavior from parents
What This Tells Us
- Risk factors are not a moral failing or a lack of willpower. They’re patterns and circumstances that make the brain more vulnerable to using substances as a coping mechanism.
- The more you understand your own risks, the easier it is to make changes that help keep things in balance.
- This is also why personalized support matters in treatment and recovery. What triggered one person’s addiction might be completely different from someone else’s.
If You’re Worried About Yourself
If you’ve noticed signs that your substance use feels harder to control, or that you’re turning to it more often as a way to cope, it might be time to talk to someone. You don’t need to wait for things to hit rock bottom. Getting support early can prevent long-term damage and make recovery feel more manageable. Contact us today.
FAQs About Heredity and Addiction
If addiction is genetic, why doesn’t everyone in the same family struggle with it?
Genetics influence risk, not outcomes. Even in the same family, people have different personalities, stress levels, support systems, and life experiences. One sibling might turn to substances to cope with anxiety, while another finds healthier outlets. Genetics can make addiction more likely, but individual choices and environments shape the results.
Are behavioral addictions (like gambling or sex addiction) hereditary too?
Yes, there’s evidence that behavioral addictions may also run in families. These behaviors affect similar reward systems in the brain as drug and alcohol use. If you have a family history of addiction, substance-related or behavioral, you may have a higher risk of developing similar patterns.
Can someone grow out of a “genetic predisposition” if they never start using substances?
While you can’t change your genes, you can lower your risk by building strong coping skills and avoiding early exposure. If you never start using addictive substances in the first place, or find healthy ways to manage stress and emotions, you can avoid triggering that genetic vulnerability.
Does the type of substance matter when it comes to family history?
Sometimes. You may be more sensitive to the same substances your relatives used, especially if there’s a pattern of alcohol, opioids, or stimulants in the family. But a family history of one type of addiction can also increase risk for others, because the underlying vulnerability is more about brain chemistry than the substance itself.