Did you know that certain drug interactions can increase your chances of developing a potentially-lethal set of symptoms known as serotonin syndrome? Knowing which medications, over-the-counter remedies, supplements, and drugs of abuse put you at risk may just save your life.
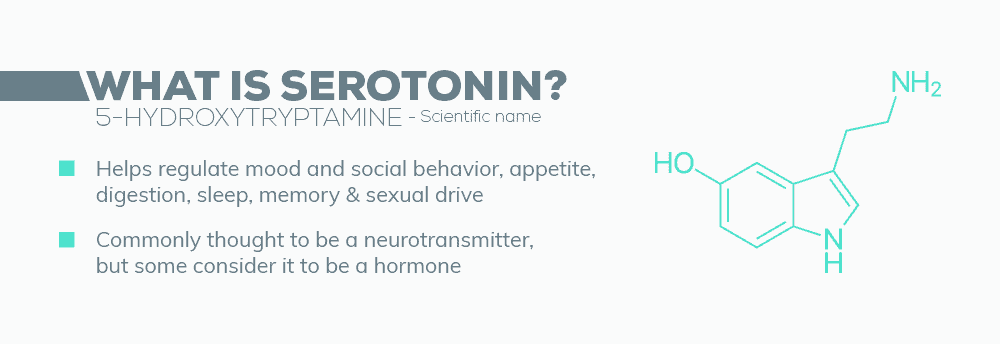
First Things First—What is Serotonin?
Serotonin is a neurotransmitter, which means it helps relay messages between different regions of the brain. It is closely associated with many different areas of physical and mental health, including:
- Mood
- Memory
- Sleep
- Sexual Desire/Function
- Learning
- Appetite
- Social Behavior
- Temperature Regulation
- Cardiovascular Function
- Muscle Performance
- Endocrine System
- Bowel Function
- Clotting
Up to 90% of the body’s serotonin is found in the gastrointestinal tract. Interestingly, although serotonin is manufactured in the both GI tract and the brain, it cannot pass through the blood-brain barrier. This means that the serotonin used by the brain must be produced there. This also means that while serotonin blood levels can be measured, there is no corresponding test to measure the amount of serotonin in a person’s brain. If there is any kind of imbalance, it is best detected through other signs and symptoms.
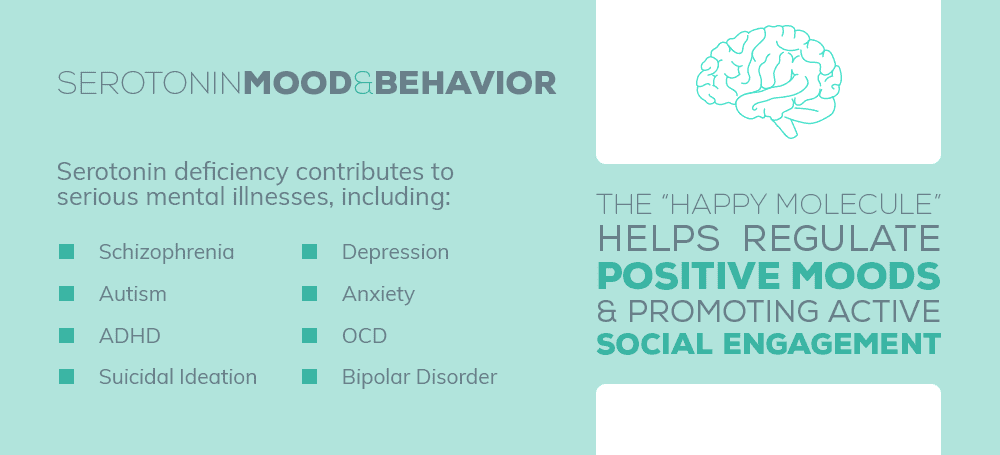
Serotonin, Mood, and Behavior
“Serotonin imbalance has long been linked to a variety of psychiatric disorders, including depression, bipolar disorder and schizophrenia…” ~ Dr. Tom Maniatis, Ph.D., Columbia University Serotonin is known as the “happy molecule” because of the role it plays in regulating positive moods and promoting active social engagement. Having the proper levels of serotonin is a key aspect of good overall brain health. But the opposite is also true – a serotonin deficiency can be linked to any or all of these serious mental illnesses, including:
- Depression—Of special relevance, women produce 52% less serotonin than men, and hormone levels fluctuate during menstruation. This helps explain why women are twice as likely as men to be diagnosed with depression.
- Anxiety—Both low AND high serotonin levels contribute to anxiety.
- Intermittent Explosive Disorder – Affecting the amygdala and characterized by extreme and uncontrollable outbursts of violence.
- Bipolar Disorder
- Schizophrenia
- Obsessive-Compulsive Disorder
- Autism—Up to 30% of autistic patients have low levels of serotonin.
- ADHD—The children of mothers with serotonin deficiencies are up to 2.5 times more likely to be diagnosed with a hyperactivity disorder.
- Suicidal Ideation–reduced serotonin can “result in impaired inhibition and a greater propensity to act on powerful feelings such as suicidal or aggressive feelings”.
What Causes Serotonin Deficiency?
There are several reasons why someone might have low levels of serotonin in their brain.
- Alcohol
- Anger
- Aspartame
- Caffeine
- Diabetes or insulin resistance
- Diet Pills
- Digestion problems
- Ecstasy
- Genetics
- Hormone imbalances (adrenal, estrogen, thyroid)
- Hypoglycemia
- Inflammation
- Infections
- Lack of exposure to sunlight
- Malnutrition
- Medication
- Nutritional deficiencies
- Poor exercise
- Problems converting tryptophan to Serotonin
- Smoking
- Stress
How Serotonin Deficiency is Linked to Substance Abuse
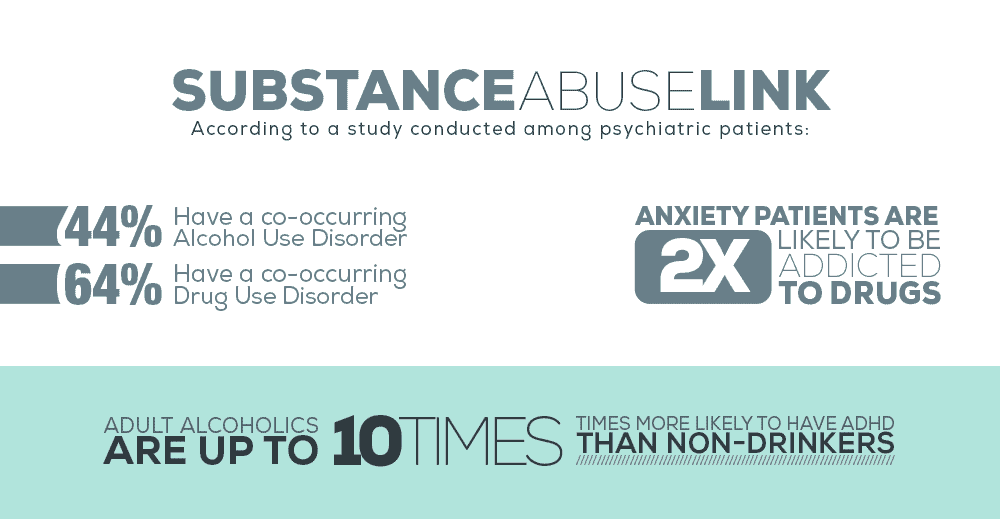
“The higher the serotonin levels someone has, the less likely they will become addicted.” ~ Dr. Sarah Bradbury, Ph.D., Victoria University of Wellington Serotonin levels play a complicated cyclical role in the development of an addictive disorder. There is a strong connection between mental illness and addiction. According to a study conducted among psychiatric patients:
- 44% have a co-occurring Alcohol Use Disorder (AUD)
- 64% have a co-occurring Drug Use Disorder
And when you consider some of the specific psychiatric conditions linked to low serotonin levels, the connection between that deficiency and subsequent substance abuse becomes more apparent:
- AUD Patients—64% have depression
- Anxiety patients are twice as likely to be addicted/dependent on drugs.
- Cannabis use is a factor in 80% of schizophrenia cases.
- 56% of people with bipolar disorder abuse alcohol and/or drugs.
- More than 1 in 4 people with OCD meet the lifetime criteria for an addictive disorder.
- Adult alcoholics are up to 10 times more likely to have ADHD than non-drinkers.
There are three possible explanations for the comorbidity of low serotonin, mental illness, and addiction. FIRST, there may be a genetic link that predisposes someone to all three conditions—each would then play a part in the development of and the worsening of the others. SECOND, decreased serotonin activity can result in an impaired ability to plan, delay gratification, or control impulses. This means that a person with a serotonin is less biologically able to resist drug cravings. THIRD, when a person who is already genetically vulnerable to addiction also suffers from co-occurring serotonin deficiency and mental illness, they often attempt to self-medicate to alleviate the uncomfortable emotional symptoms of those conditions.
Serotonin Syndrome – Another Name for Neurotransmitter Toxicity
And while using drugs or alcohol may make them feel better temporarily over the short-term, regular substance use progresses to substance abuse and addiction far too quickly and easily. Even worse, self-medicating when there is a serotonin imbalance can result in the rapidly-presenting and potentially-deadly symptoms of serotonin syndrome. Serotonin syndrome is a reaction to certain prescription medications, supplements, or illicit drugs that results in toxic levels of serotonin within the brain. In the case of legitimately-prescribed medications, the reaction can be triggered even when they are taken as directed. There is no laboratory test that can confirm serotonin syndrome. The condition is diagnosed based upon the patient’s history of drug/medication use, physical examination, and any presenting symptoms. This method is up to 97% accurate.
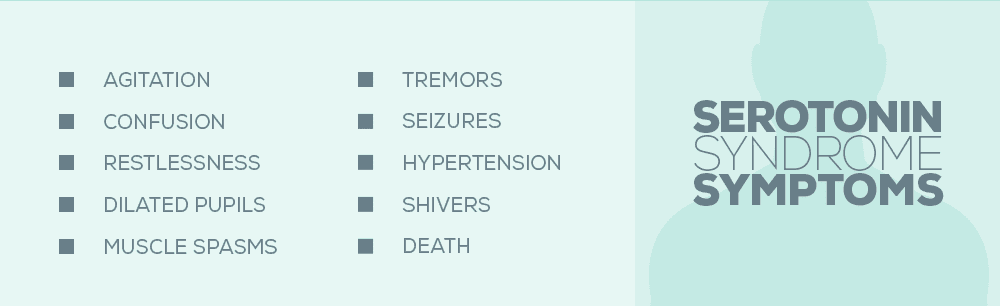
What Are the Symptoms of Serotonin Syndrome?
Again, serotonin syndrome is a drug reaction, occurring after a new drug or a new dosage level is taken. Symptoms typically begin rapidly—6 to 24 hours after consumption.
- Agitation
- Confusion
- Restlessness, often to the point of feeling the need to be in constant motion
- Extreme aggressiveness
- Dilated pupils
- Jerky movement of the eyes
- Extremely sensitive reflexes
- Muscle spasms
- Uncontrollable twitches
- Tremors
- Full-body seizures
- Accelerated heartbeat
- High blood pressure
- Abnormally dry mouth
- Shivering
- Sweating
- High fever – over 104°
- Increased bowel sounds
- Diarrhea
- DEATH
What Is the Treatment for Serotonin Syndrome?
The first step in treating serotonin syndrome is to discontinue use of the causal drug. If the triggering substance is discontinued, mild cases of serotonin poisoning will go away on its own within 1 to 3 days. However, in more serious cases of serotonin syndrome, hospitalization may be necessary. The next step is to administer a serotonin-inhibiting medication, such as:
- Alosetron
- Carbinoxamine
- Chlorpromazine
- Cilansetron
- Clozapine
- Cyproheptadine
- Dolasetron
- Fenclonine
- Feverfew
- Granisetron
- Hydroxyzine
- Ketanserin
- Metergoline
- Methdilazine
- Methysergide
- Mianserin
- Mitrazapine
- Nefazodone
- Ondansetron
- Oxatomide
- Oxetorone
- Palonosetron
- Pizotifen
- Promethazine
- Propranolol
- Quetiapine
- Reserpine
- Risperidone
- Ritanserin
- Spiperone
- Trazodone
- Tropisetron
The priority during treatment for serotonin is to regulate those symptoms that are life-threatening – hyperthermia, tachycardia, autonomic dysfunction, and seizures. Decontamination with activated charcoal may be necessary, as well as the administration of tranquilizers, sedatives, antihypertensive drugs, or even “flight-or-flight” hormones such as epinephrine or norepinephrine. Importantly, physical restraints are not recommended for serotonin poisoning patients who are severely agitated or delirious. Straining against those restraints forces muscle contractions that cause a dangerous buildup of lactic acid and increased body temperature. Patients using drugs with a long half-life or extended duration of action can experience symptoms up to two weeks, and muscle pain and weakness may persist for months.
SSRIs and Serotonin Syndrome
Serotonin reuptake inhibitors (SSRIs) are a class of antidepressants that increase the serotonin levels by limiting reabsorption. Although primarily prescribed for major depression, SSRIs are also given for anxiety, OCD, PTSD, panic disorder, anorexia, bulimia, and chronic pain. They are the most-widely prescribed type of antidepressant. Serotonin syndrome occurs in approximately 15% of SSRI overdoses. Examples of SSRI medications include:
- Citalopram (Celexa)
- Dapoxetine (Priligy)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Fluvoxamine (Luvox)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
SNRIs and Serotonin Syndrome
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs), are a class of antidepressants that work by blocking the reabsorption of the neurotransmitters serotonin and norepinephrine, thereby increasing their levels. SNRIs can also be prescribed for anxiety, OCD, ADHD, fibromyalgia syndrome, chronic pain, and for the relief of severe menopausal symptoms. Abrupt discontinuation of SNRIs is not recommended because it can trigger withdrawal symptoms. Examples of SNRIs include:
- Atomoxetine (Strattera)
- Desvenlafaxine (Desfax, Ellefore, Pristiq)
- Duloxetine (Cymbalta)
- Levomilnacipran (Fetzima)
- Milnacipran (Dalcipran, Ixel, Savella, Toledomin)
- Tramadol (Ultram)
- Venlafaxine (Effexor) – the most-commonly-used SNRI
Substances to Avoid When Taking SSRIs and SNRIs
Some OTC pain relievers – aspirin, ibuprofen, and naproxen – interfere with the efficiency of these medications, and even worse, increase the risk of gastrointestinal bleeds. There are also a number of substances that, when used with SSRIs and SNRIs, may trigger serotonin syndrome. What is particularly concerning about this list is how many different conditions they treat:
- Bupropion (Wellbutrin, Zyban) – anti-smoking medication
- Buspirone – prescribed for anti-anxiety
- Carbamazepine (Tegretol) – prescribed for migraines
- Cyclobenzaprine (Flexeril) – a muscle relaxant
- Dextromethorphan – an ingredient in many OTC cough suppressants, and an extremely-popular drug of abuse
- Droperidol (Inapsine) – for anti-nausea
- Ginseng – herbal supplement taken for memory, diabetes, fatigue, and menopause symptoms.
- Linezolid – prescribed for MRSA and other antibiotic-resistant infections
- Lithium – prescribed for bipolar disorder or major depression when other antidepressants don’t work
- MDMA (Ecstasy) –the illicit drug of choice the rave/party culture, abused for its stimulant and euphoriant effects
- Metoclopramide (Reglan) – for anti-nausea
- Mirtazapine – prescribed for both anxiety and depression
- Monoamine Oxidase Inhibitors (MAOIs) – often considered the “last line of defense” against depression, MAOIs are typically prescribed when other medications are ineffective
- Methylene Blue
- Moclobemide
- Phenelzine
- Selegiline
- Tranylcypromine
- Nutmeg – herbal supplement taken for brain health, blood pressure, and circulation
- Ondansetron (Zofran)—for anti-nausea
- Pethidine/Meperidine (Demerol) – a synthetic opioid pain medication
- Ritonavir (Norvir) – anti-retroviral medication given to treat HIV/AIDS
- Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) – (more in the next section)
- St. John’s Wort – A medicinal herb popularly taken as an OTC supplement for depression
- Tramadol – a prescription opioid pain medication
- Tricyclic Antidepressants (TCAs) – an older generation of antidepressant/mood disorder medications
- Triptans (Amerge, Axert, Imitrex) – prescribed for migraines or cluster headaches
- Valproic Acid (Depakene) – given for migraines
- Yohimbe – a dietary supplement sold as an aphrodisiac
Who Shouldn’t Take SSRIs and SNRIs?
People with certain pre-existing conditions should avoid SSRIs and SNRIs:
- High blood pressure
- Chronic alcoholism
- Liver disease
- Coronary artery disease
- Anorexia
- Bulimia
- Glaucoma
These medications should NEVER be taken within 24 hours of another antidepressant, because it may result in a serotonin overdose.
Opioids and Serotonin Syndrome
“Patients and practitioners should be aware that opioid analgesic use of longer than 30 days imposes risk of new-onset depression.” ~Dr. Jeffrey Scherrer, Ph.D., Associate Professor for Family and Community Medicine, St. Louis University People who suffer pain lasting longer than 6 months have a more than quadrupled risk of depression than those not in chronic pain, according to the Journal of American Medicine. And, among opioid abusers who have switched to cheaper, easier-to-get heroin, the likelihood becomes even greater. Approximately 48% of heroin addicts also experience co-occurring depression. But when a person uses heroin or takes opioid painkillers like Vicodin, OxyContin, or codeine in combination with certain serotonergic medications, the risk of serotonin poisoning increases dramatically. There are two prevailing theories as to why the interaction between opioids and antidepressants increases the likelihood of serotonin syndrome. The first theory is that even alone, opioids act as inhibitors that prevent serotonin reabsorption. When combined with other inhibitors, the effect is magnified. Secondly, opioids impact the production of GABA, another neurotransmitter, and as a result, access serotonin is released. In addition, while some opioids – specifically, buprenorphine, hydromorphone, oxycodone, and oxymorphone – are not reuptake inhibitors, they still increase serotonin levels by some as-yet-undiscovered mechanism. Among all opioids, fentanyl has been linked to serotonin syndrome most often, followed by oxycodone and methadone. In 2016, the potentially-dangerous interaction between opioids and serotonergic substances caused the FDA to require drug manufacturers to make changes to the warning labels on opioid medications.
ADHD Medications and Serotonin Syndrome
ADHD medications treat hyperactivity by balancing out serotonin and dopamine levels within the brain. However, when taken in combination with SSRIs, SNRIs, or other serotonergic drugs, those levels can become toxic. Prescription ADHD drugs include:
- Adderall
- Ritalin
- Vyvanse
- Concerta
Abused Substances and Serotonin Syndrome
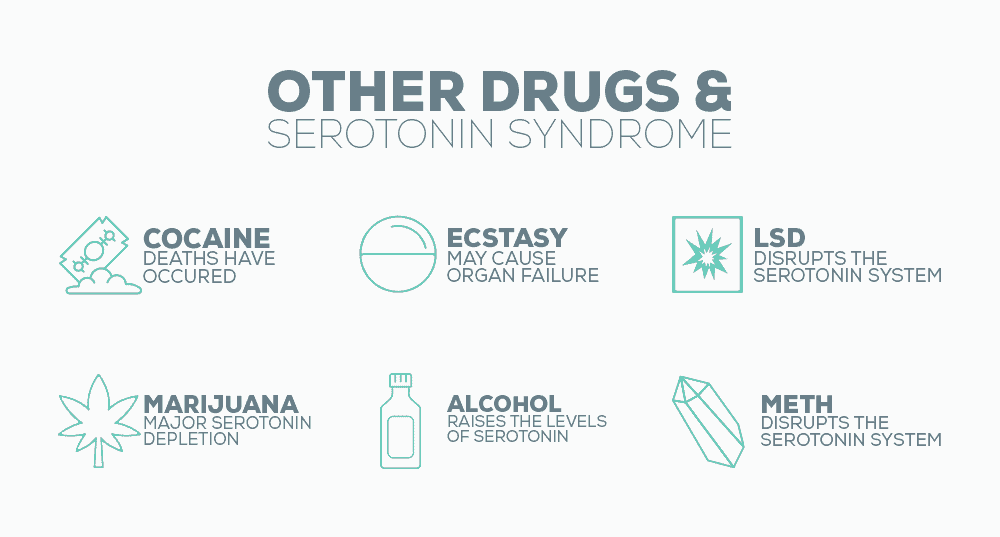
The abuse of illegal drugs can also have a significant impact on the serotonin levels within the brain. Besides the aforementioned heroin, other drugs that can contribute to serotonin syndrome include:
- Cocaine –Fatalities have been reported
- Ecstasy – Can cause multi-organ failure
- LSD – This potent hallucinogen disrupts the serotonin system
- Methamphetamines – Especially at high doses
- Marijuana—At low doses, marijuana increases serotonin levels. Paradoxically, at high doses, it causes a major serotonin depletion, making it more likely the user will need antidepressants. It is also important to note that when marijuana is smoked it is difficult to accurately measure the dosage.
- Alcohol—Drinking alcohol temporarily raises serotonin levels—raising the odds of serotonin syndrome—but chronic alcoholism causes a deficiency that can dramatically worsen depression.
What Does All of this Mean?
The first takeaway is that serotonin syndrome is a serious, potentially life-threatening condition that should not be ignored. When symptoms manifest, serotonin syndrome can rapidly turn into an emergency, so medical help should be sought immediately. Serotonin syndrome is almost completely avoidable, and communication is the best tool you have at your disposal. ALWAYS be completely open and honest with your doctor about any medications, supplements, OTC remedies, and drugs you are taking – legal or not. Your doctor is not there to judge you, and omitting anything could jeopardize your health. At the same time, depression is also not to be taken lightly, especially if it co-occurs with a substance abuse disorder. To find just the right balance of medication, therapy, and lifestyle changes that will help you successfully manage both conditions, you need the help of an experienced staff of professional specialists.
What Did you Think About This Blog?
Give it a Rating!