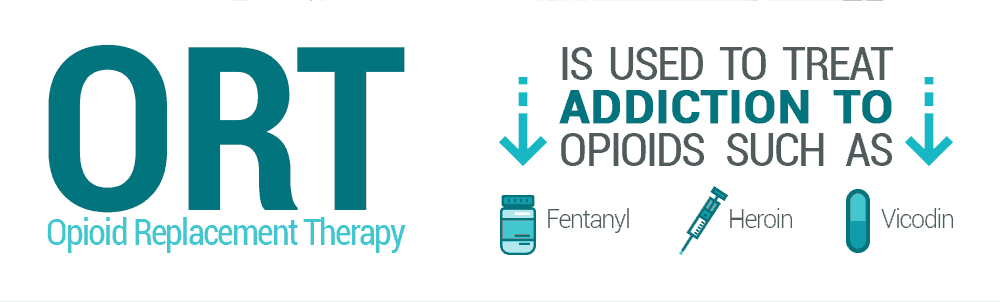
For the past 70 years, people addicted to opioids such as illicit heroin or prescription painkillers have been treated via Opioid Replacement Therapy (ORT), historically using methadone, and, increasingly, Suboxone pills. But even though this newer medication is starting to supplant methadone as the “go-to” ORT medication of choice, some people are still largely unaware of what Suboxone is, why Suboxone is a viable alternative to methadone, or where to find Suboxone doctors.
First Things First—What is Opioid Replacement Therapy?
“It gives the user a better chance in the long-term to beat the psychological obsession linked to addiction.” ~ Karen Griessel, social worker ORT is when, under strict medical supervision, the abused opioid – OxyContin, Vicodin, fentanyl, heroin, etc. – is discontinued, and then replaced with another safer opioid medication – typically methadone or a buprenorphine-based medication such as Suboxone or Subutex. Because these prescription drugs don’t deliver such a potent “high”, there is much less potential for abuse. ORT is a process. Once the medication has been substituted for the opioid of abuse, the long-term goal is to very slowly reduce the dosage until the cravings have subsided enough for the person can resist cravings on their own. When complete abstinence is the goal, ORT is best used in conjunction with a more comprehensive recovery program that includes education, counseling, group therapy, and life-coaching skills. But with serious opioid addiction, sometimes total abstinence just isn’t a realistic current goal. In these cases, the focus becomes harm reduction, to both the individual and to society as a whole.
“We offer medical detox and rehabilitation and take many health insurance plans. Take a look at our 28 day program.”
“A motivated patient on replacement therapy can make astounding changes in a year. Many change careers, go back to school, and turn their lives around to where they might have been before they started taking drugs. I’ve seen miracles happen.” ~ Dr. Logan Graddy, MD, a neurologist in Durham, North Carolina, who advocates for ORT For some people, ORT is a controversial subject, because they believe that it merely swaps one addiction for another. However, statistics show that ORT can have multiple benefits:
- Approximately two-thirds of opioid addicts who receive OTR are able to completely abstain from illicit opioid misuse.
- Of special significance, 70%-95% are able to significantly reduce their illicit opioid use, resulting in:
- Fewer cases of hepatitis and HIV caused by the sharing of contaminated needles
- Reduction in suicide
- Lower crime rate
- Less imprisonment
- Higher rates of employment
- Continuity of care
- Greater exposure to comprehensive drug treatment programs
Compared to the economic impact of opioid addiction to society, ORT is extremely cost-effective. As far back as 1991, the National Institute on Drug Abuse estimated the annual cost to maintain an opioid addict:
- Untreated and on the street – $43,000
- In prison – $34,000
- A residential drug-free program – $11,000
- ORT – $2400
When you adjust those 1991 figures to reflect the costs in 2017, the cost-effectiveness becomes even more apparent.
What is Suboxone?
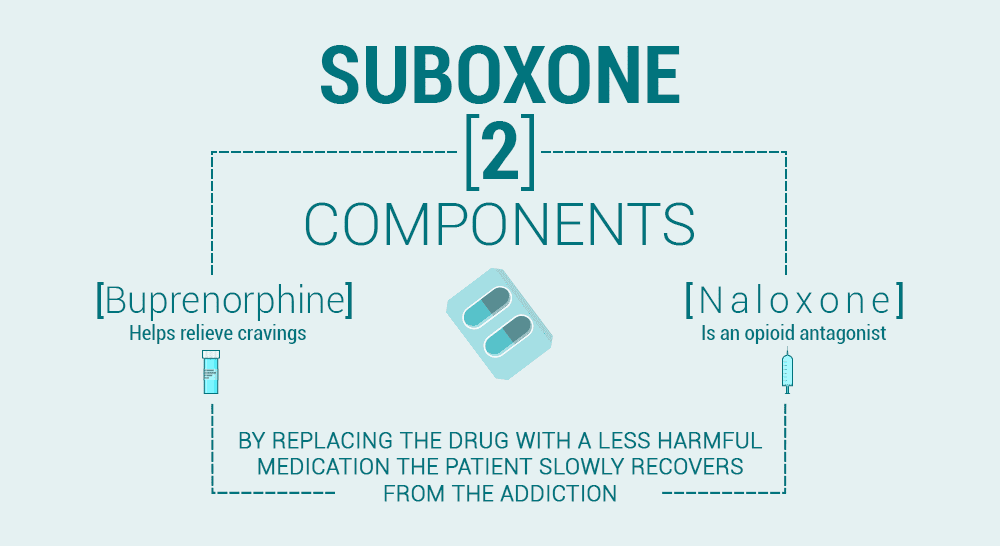
“They are then able to take a medicine once a day that they know will protect them from overdose, protect them from withdrawal and allow them to engage in their normal activities. And I think that’s the transformative element of Suboxone.” ~Dr. Grant Scull, Kaiser Permanente Suboxone is a first-line treatment for opioid addiction. It works by blocking the brain’s receptors while still partially activating them – thereby reducing both cravings and withdrawal symptoms. Suboxone is a combination drug, composed of buprenorphine and naloxone. Each individual component has a specific purpose:
- Buprenorphine – helps eliminate cravings for opioids by partially blocking the brain’s opioid receptors. Similar to other opioids like heroin, buprenorphine interacts directly with the brain’s opioid receptors – more specifically the mu opioid receptors. But rather than activating them fully like other powerful opioids, buprenorphine does so to a much smaller degree.
Even other ORTs like methadone are considered full agonists, making them much more likely to become substances of abuse than buprenorphine. As a result, Suboxone doctors have substantially more flexibility when it comes to prescribing when compared to methadone clinics.
- Naloxone – a chemical deterrent included to prevent abusing Suboxone intravenously rather than taking it properly. Naloxone is most commonly used to help reverse opioid overdoses. In a sense, this drug kicks off other opioid molecules from the opioid receptors and takes their place immediately, thus quickly reversing the effects that these drugs can have on the body.
However, when naloxone does remove these opioid molecules, it puts users in a state of “precipitated withdrawal,” which is characterized by the incredibly uncomfortable symptoms of opioid withdrawal almost immediately. When taken properly, however, this compound is rendered ineffectual. Suboxone used to come in the form of a dissolvable pill that patients simply placed under their tongue, but the abuse potential of this form was far too high. As a result, manufacturers instead opted for a buccal, sublingual, or transdermal patch to administer the drug, making it harder for individuals to abuse it.
Comparing Methadone and Suboxone
“Suboxone has been a godsend for us in addiction medicine.” ~ Dr. Lloyd Westby, a Pentiction family doctor specializing in addiction treatment Since 1947, the first-line prescribed medication for opioid addiction was methadone, but with the introduction of Suboxone in 2002, more and more doctors are making a switch. Suboxone has several advantages over methadone, including:
- Produces less of a “high” than methadone, limiting its desirability as a potential drug of abuse. The euphoria is less intense because Suboxone is so long-lasting, with a duration of effects of between 24 and 72 hours.
(Methadone’s pain-relieving effects only last 4-8 hours)
- Has a “ceiling affect” – this means that taking more of the medication will not increase the intoxication/euphoria.
(Every year, thousands of patients overdose while trying to get high on methadone.)
- Causes less respiratory depression than methadone, thereby lowering the risk of overdose.
(Between 1999 and 2007, fatal methadone overdoses in the United States rose sevenfold.)
- Can be prescribed as a take-home medication.
(Methadone patients must make a daily trip to the doctor or clinic.)
- Is less likely to trigger sexual side effects.
(At least 14% of male methadone patients experience sexual dysfunction)
- Suboxone can also treat depression and neonatal abstinence syndrome. The length of treatment is 40% shorter and the hospital stay is 24% shorter when opioid-dependent infants are given buprenorphine instead of morphine.
What Are Some Suboxone Side Effects?
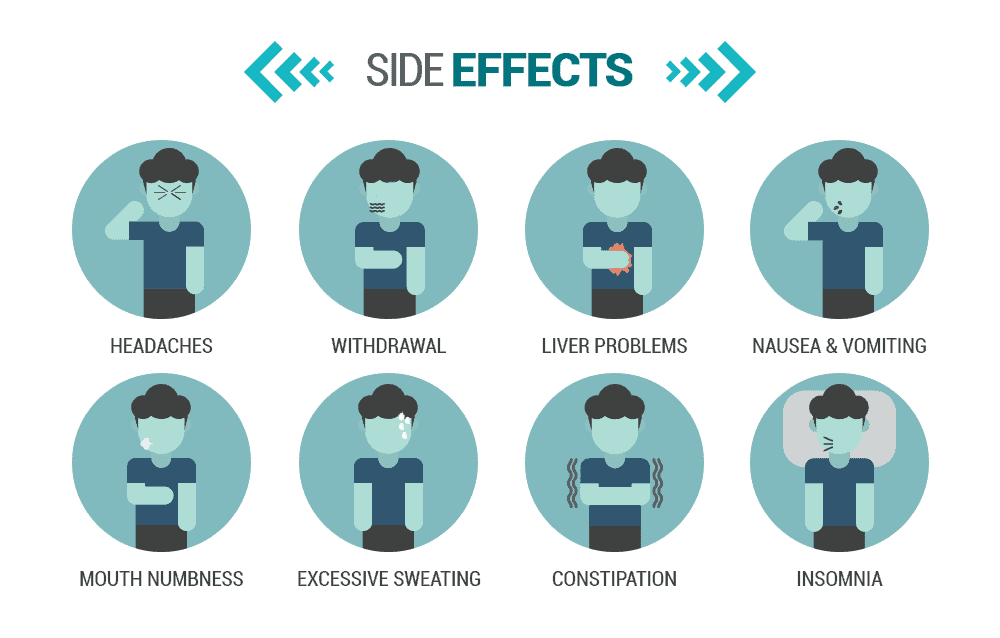
Suboxone is an opioid medication, so there are several serious potential side effects, especially if you are taking other medications that contain opioids or benzodiazepines. Your Suboxone doctor will go over some of these side effects with you and inform you of the warnings involved before starting your Suboxone treatment.
- Respiratory depression, to the point of coma or death
- Liver problems
- Decreased blood pressure
- Allergic reactions
- Opioid withdrawal
- Physical dependency
- Potential for abuse
- Impaired coordination
- Sleepiness
Less-serious common side effects include:
- Nausea and/or Vomiting
- Headache
- Blurred vision
- Excessive sweating
- Painful and/or swollen tongue
- Numbness in the mouth
- Unusually-red mouth
- Heart palpitations
- Constipation
- Back pain
- Impairment inability to pay attention
- Lightheadedness
- Mild intoxication
- Insomnia
Can My Family Doctor Prescribe Me Suboxone?
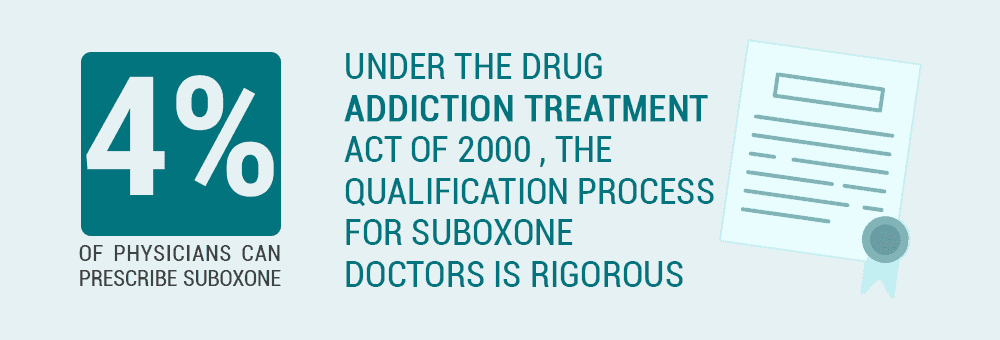
Probably not. Although almost every doctor in America can prescribe painkilling opioids such as OxyContin, Vicodin, or fentanyl, the vast majority of doctors are NOT permitted to prescribe Suboxone or other medications containing buprenorphine. Buprenorphine is a tightly-controlled medication, and doctors must have a special certification in order to prescribe or dispense it to their patients. In fact, according to the National Alliance of Advocates for Buprenorphine Treatment (NAABT), only a bit over 35,000 out of 800,000 U.S. physicians have the necessary credentials to prescribe buprenorphine for addiction. That’s only around 4% of active physicians today. As you can see, then, finding Suboxone doctors near you can be especially tough.
Why Aren’t There More Suboxone Doctors Near Me?
“What is a concern to me is that more physicians don’t feel the responsibility to step up (and get a license to provide buprenorphine).” ~ Melinda Campopiano, Chief Medical Officer at Health and Human Services’ Center for Substance Abuse Treatment Under the Drug Addiction Treatment Act of 2000 (DATA 2000), the qualification process for Suboxone doctors is rigorous. State-licensed doctors wanting to disperse medications containing buprenorphine must first register with the Drug Enforcement Agency, and then meet at least one of the following criteria:
- Have an American Board of Medical Specialties subspecialty certification in Addiction Psychiatry.
- Have an American Society of Addiction Medicine addiction certification.
- Have an American Osteopathic Association subspecialty board certification in Addiction Medicine.
- Complete at least 8 hours of specialty training through programs recognized by the Substance Abuse and Mental Health Services Administration.
- Suboxone doctors must have other training or experience that demonstrates the physician’s ability to treat and manage patients with opioid dependency according to their state’s medical licensing board.
- A prescribing Suboxone doctor must have other training or experience that demonstrates the physician’s ability to treat and manage patients with opioid dependency according to the U.S. Department of Health and Human Services.
After SAMSHA has verified the doctor’s background and training, the DEA will assign a special identification number. Every time that Suboxone doctor writes a prescription for buprenorphine, they must include both this special number and their regular DEA registration number.
What Medications Contain Buprenorphine?
Medications containing buprenorphine include Suboxone, Subutex, Bunavail, Zubsolv, and Probuphine. Probuphine is a buprenorphine-only implant that “provides steady, continuous levels of buprenorphine from 4 soft, flexible, 1-inch rods. It can be inserted in your doctor’s office.” Bunavail and Zubsolv are sublingual drug combinations containing both buprenorphine and naloxone, similar to Suboxone. Subutex is a medication containing only buprenorphine, without the naloxone abuse deterrent. The lack of an abuse-deterrent is one of the reasons cited for Subutex being taken off of the market in 2011. It also came in the form of a pill as well, making it easier for patients to crush, snort, or inject Subutex in order to feel high. As a result, finding Subutex doctors today is harder. Suboxone was also marketed as a pill up until 2012. However, concerns over pediatric exposure to the drug spurred producer Reckitt Benckiser – a major British pharmaceutical manufacturer – to find a new method of administration. As such, Suboxone doctors now prescribe a sublingual or buccal patch to deliver the drug instead.
Can Buprenorphine Be Abused?
Like any other opioid, buprenorphine can in fact become a substance of abuse. While the risk of addiction is significantly lower than with other drugs such as heroin, OxyContin, and the notorious fentanyl, buprenorphine uses the very same cellular structures and pathways as these drugs. Consequently, dependency and eventual addiction are both risks. The special prescribing certifications, the embedded naloxone, and the “ceiling effect” all make abuse far less likely though. Unfortunately, individuals looking to get high have found out how to get Suboxone without a doctor or use the substance illicitly. There are a couple of ways this can happen. First, they may simply find a Suboxone doctor and rob their clinic, stealing the valuable drug in the process. According to StreetRx which purports to show the latest street prices for prescription drugs, a single dose of Suboxone film can run anywhere from $10 to $25. And when you include generic versions, doses can bring in up to $60 a piece. The more likely scenario, however, is that they got their hands on this drug by using what’s been called a “pill mill.” These clinics tend to have exceptionally loose prescribing guidelines and Suboxone doctors in these clinics will typically overprescribe their patients. Many of these facilities also operate on a cash-only basis, making the operations even harder to track legally. These especially accessible prescriptions can also end up making their way onto the black market. Drug dealers have even created elaborate systems where they are willing to sponsor patients’ visits to these clinics in exchange for a hefty proportion of the prescription written by the Suboxone doctor.
Are There Federal Patient Limits for Suboxone Doctors?
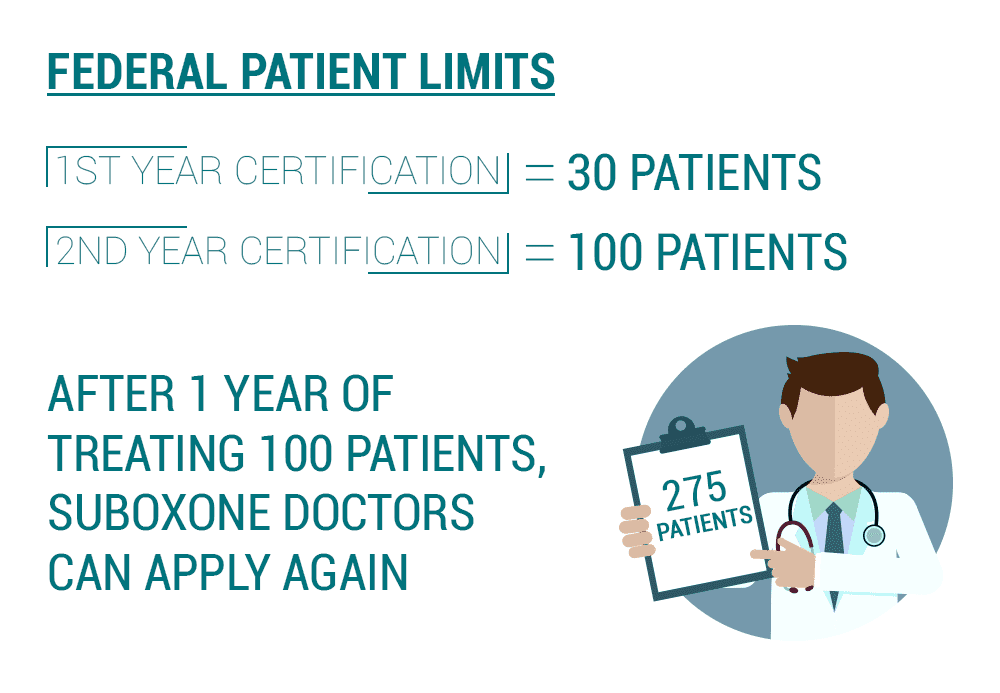
In addition to the educational and experiential requirements, even after the certification is granted, Suboxone doctors are limited to the number of buprenorphine patients they may have in an opioid dependence treatment program. As mandated by DATA 2000, individual Suboxone doctors may not treat more than 30 patients at a time for opioid dependence during the first year of certification. After that first year, doctors prescribing Suboxone can submit a request for authorization to treat 100 patients at a time. Under new suboxone laws, after an additional year of treating 100 patients, Suboxone doctors can apply again, this time to have their limit increased to 275 patients at a time.
How Many Suboxone Doctors are in Each State?
SAMHSA tracks qualified providers in each state/territory. Patients can use this information to find a Suboxone doctor locally. As of 2017, here are the number of 30-patient and 100-patient certified Suboxone doctors:
- Alabama – 30 (58): 58/100 (32)
- Alaska – 30 (55)/100 (4)
- American Samoa – ZERO certified Suboxone doctors
- Arizona – 30 (192)/100 (29)
- Arkansas – 30 (19)/ 100 (6)
- California – 30 (726)/100 (80)
- Colorado – 30 (181)/100 (22)
- Connecticut – 30 (232)/100 (31)
- Delaware – 30 (24)/100 (3)
- District of Columbia – 30 (47)/100 (2)
- Federated States of Micronesia – ZERO certified Suboxone doctors
- Florida – 30 (288)/100 (61)
- Georgia – 30 (94)/100 (26)
- Guam– ZERO certified Suboxone doctors
- Hawaii – 30 (28)/100 (3)
- Idaho – 30 (48)/100 (5)
- Illinois – 30 (198)/100 (29)
- Indiana – 30 (187)/100 (32)
- Iowa – 30 (25)/100 (3)
- Kansas – 30 (34)/100 (4)
- Kentucky – 30 (166)/100 (36)
- Louisiana – 30 (71)/100 (20)
- Maine – 30 (172)/100 (17)
- Marshall Islands – ZERO certified Suboxone doctors.
- Maryland – 30 (265)/100 (33)
- Massachusetts – 30 (473)/100 (63)
- Michigan – 30 (133)/100 (15)
- Minnesota – 30 (120)/100 (10)
- Mississippi – 30 (39)/100 (6)
- Missouri – 30 (77)/100 (14)
- Montana – 30 (29)/100 (2)
- Nebraska 30 (25)/100 (1)
- Nevada – 30 (59)/100 (5)
- New Hampshire – 30 (114)/100 (20)
- New Jersey – 30 (221)/100 (16)
- New Mexico – 30 (117)/100 (11)
- New York – 30 (765)/100 (66)
- North Carolina – 30 (278)/100 (32)
- North Dakota – 30 (12)/100 (2)
- Northern Mariana Islands – ZERO certified Suboxone doctors
- Ohio – 30 (433)/100 (79)
- Oklahoma – 30 (47)/100 (11)
- Oregon – 30 (191)/100 (15)
- Pennsylvania – 30 (409)/100 (109)
- Puerto Rico – 30 (11)/100 (11)
- Republic of Palau – ZERO certified Suboxone doctors
- Rhode Island – 30 (79)/100 (15)
- South Carolina – 30 (90)/100 (10)
- South Dakota – 30 (14)/100 (1)
- Tennessee – 30 (63)/100 (47)
- Texas – 30 (223)/100 (39)
- Utah – 30 (114)/100 (19)
- Vermont – 30 (57)/100 (7)
- Virgin Islands – 30 (1)/100 – ZERO
- Virginia – 30 (174)/100 (34)
- Washington – 30 (410)/100 (27)
- West Virginia – 30 (65)/100 (18)
- Wisconsin – 30 (115)/100 (10)
- Wyoming – 30 (10)/100 (3)
Because the regulation is so new, as of yet, there are no doctors listed with a 275-patient authorization.
Examples of Local Suboxone Doctor Numbers
It’s one thing to know how many doctors who prescribe Suboxone are in a particular state, but that doesn’t tell the whole story. There are two sides to the problem – larger urban areas naturally tend to have more specialists, than less-populated rural areas, and this would include Suboxone doctors. But on the other hand, due to the fact that doctors are restricted in the number of ORT patients they can treat at one time, Suboxone doctors in urban areas might have lengthy waiting lists. To see how this might play out, let’s look at 3 different states with different levels of Suboxone providers.
- Compared to most other states, Idaho has relatively few doctors who will prescribe Suboxone.
The largest city in Idaho is Boise, with a Metropolitan population of approximately 677,000 residents. Yet there are only 13 currently-licensed and compliant Suboxone doctors within 50 miles of Boise’s most-populous ZIP Code, 83709.
- In terms of the number of doctors who prescribe Suboxone, Colorado falls somewhere in the middle.
The largest city in Colorado is Denver, with a Metropolitan population of approximately 2.8 million residents. Because it is one of the largest metropolitan areas in the country, there are 48 currently-licensed and compliant Suboxone doctors within 10 miles of Denver’s most-populous ZIP Code, 80219.
- Washington State has more Suboxone doctors than most other states.
The largest city in Washington is Seattle, with a Metropolitan population of over 3.8 million residents. Yet, even with 900,000 additional residents, there are only 3 more currently-licensed and compliant Suboxone doctors within 10 miles of Seattle’s most-populous ZIP Code, 98115, for a total of 51.
To find a Suboxone clinic or certified Suboxone doctors near you, you can enter your city or ZIP Code here to use the manufacturer’s Suboxone doctor locator to find the nearest Suboxone programs in your area. .
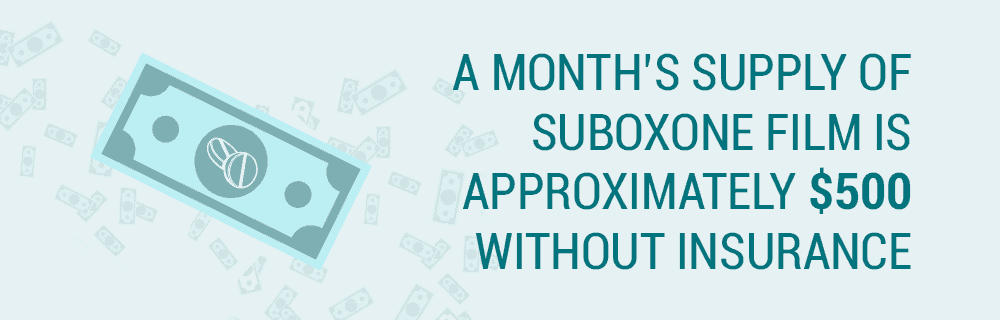
How Much Does Suboxone Cost?
According to prescribing information, the target dosage for maintenance treatment requires a single daily dose of 16mg/4 mg, which would be two sublingual strips. This means the Suboxone cost of a month’s supply of Suboxone film is approximately $500 without insurance. As with anything, however, there are ways of reducing your Suboxone cost that you may not be fully aware of.
Are There Ways to Get Suboxone Cheaper?
There are several ways to save money on Suboxone.
- Your personal insurance – Personal health insurance is typically one of the main factors in reducing Suboxone costs. Be sure to check with your provider before starting a Suboxone program though as not all insurance providers will cover treatment.
- Prescription discount plans – These plans often provide prescription medications at a reduced price whenever you refill them through a certain provider. As a result, you can see your Suboxone cost drop pretty dramatically just by using a discount plan.
- Manufacturer programs – One of the most substantial savings on your Suboxone cost may come directly from the manufacturer. This savings card offered by Indivior Inc. offers up to $75 off your copay per month if you’re using insurance and savings of more than $170 per month if you aren’t.
Does Medicare Pay for Suboxone?
Generally speaking, Medicare does not cover prescription drugs that are given on an outpatient basis. However, substance abuse treatment like Suboxone programs MAY be covered if it is medically necessary and care is provided by an outpatient or inpatient treatment center that is Medicare-certified. Even then, Medicare coverage is typically only extended when the medication was used during emergency treatment – detoxification or early stabilization. As such, your Suboxone provider costs typically will not be supplemented by Medicare.
Can I Buy Suboxone Online Without a Prescription?
No – at least, not legitimately. As you can tell from the extensive qualifications required for buprenorphine licensing, Suboxone programs are subject to extremely tight regulation. Online pharmacies offering Suboxone for sale without a prescription, or a doctor visit are neither reputable nor safe and they should be avoided at all costs.
Is Suboxone for Everyone?
There are certain circumstances where your doctor may decide against prescribing you Suboxone or any other buprenorphine medication:
- You are not motivated to recover – Because buprenorphine Suboxone is a take-home therapy, it is typically reserved for those people who truly want to recover and are therefore more likely to comply.
- You have a severe opioid addiction – Buprenorphine Suboxone is recommended for people with less-severe opioid dependency. In the worst cases of opioid addiction, methadone is the preferred treatment.
- You have an Alcohol Use Disorder – Because both buprenorphine and alcohol are central nervous system depressants, using them in combination can result in a fatal interaction, due to respiratory depression. Naloxone is also broken down by the liver and if you have already compromised this organ due to alcohol abuse, a Suboxone program may in fact be dangerous to your health.
- You use/abuse benzodiazepines or sedatives –Likewise, tranquilizing or sedating medications such as antianxiety drugs or sleeping pills can trigger a fatal interaction when used with buprenorphine Suboxone.
- You have a co-occurring mental condition – Anyone with violent, delusional, or suicidal behaviors is not an ideal candidate for take-home ORT.
- You are pregnant – For opioid-dependent people who are pregnant, methadone is the recommended treatment.
Can Buprenorphine Be Prescribed for Pain?
Yes…IF the prescribing physician specifies that it is for pain. Suboxone, Subutex, and other buprenorphine medications are often a good option for patients suffering chronic pain, but who also have a personal history of substance abuse. Transdermal buprenorphine patches –Butrans, for example – are also available. Of special reference, when these medications are prescribed for pain instead of opioid addiction, the prescriber is not required to provide the special buprenorphine or Suboxone DEA number.
What If I Need Suboxone NOW?
“Taking medication for opioid addiction is like taking medication to control heart disease or diabetes. It is NOT the same as substituting one addictive drug for another. Used properly, the medication does NOT create a new addiction. It helps people manage their addiction so that the benefits of recovery can be maintained.” ~SAMHSA, Medication-Assisted Treatment for Opioid Addiction: Facts for Families and Friends If the Suboxone doctors in your area have a waiting list because they are unable to accept new patients currently, and you need immediate help for an addiction to opioids, you have two choices. FIRST, you can travel. Other doctors in other areas may have patient availability, so if you are willing to do a little homework and a little driving, you can probably find doctors to prescribe Suboxone around you. SECOND, you can opt to temporarily use methadone as your ORT medication. Regardless of any inconvenience or preference, it is still a better and safer option than allowing your addiction to other, more dangerous opioids to continue to worsen. Ask to be put on the waiting list of the Suboxone doctor, and then get the ORT help you need. When a slot on the waiting list opens up, work with your Suboxone doctor so you can transition safely.
What’s the Bottom Line about Suboxone?
“Addressing the epidemic of opioid addiction is my highest public health priority. One element of that effort is promoting more widespread, safe adoption of MAT (medication-assisted treatment) as a way to help more people overcome addiction.” ~ Dr. Scott Gottlieb, M.D., Commissioner of the Food and Drug Administration When taken as directed, buprenorphine Suboxone is a safe and very effective medication for the treatment of opioid addiction. Its chief benefit is that it allows opioid-dependent people to achieve a level of stability that would be impossible if they were still abusing other, more dangerous drugs such as heroin, Oxycontin, or fentanyl. But it’s important to remember that, by itself, taking Suboxone is not truly recovery from addiction. That is best achieved when the medication is combined with other therapeutic strategies, such as behavioral counseling, and ongoing professional support. With a comprehensive treatment plan that addresses the disease of addiction on multiple levels, there is no reason why even the most desperate of opioid addicts can’t eventually fully recover and stand on their own, without the need for ORT medications.
What Did you Think About This Blog?
Give it a Rating!